SECTION A: RENAL ANATOMY
INTRODUCTION
Kidneys, also known as “renes” in Latin, are bean shaped organs located in our body. They function to regulate the acid base balance, maintenance of homeostasis, vitamin D3 and hemoglobin. They remove the waste products of metabolism by filtering the blood passing through. Acute or chronic derangement of kidney function can give rise to various signs and symptoms due to accumulation of these waste products and altered acid-base, electrolytes and fluid homeostasis. This chapter reviews the anatomy of kidneys and describes the physiology of urine formation, which is important to understand the basis of clinic-pathological features of renal dysfunction.
Gross Anatomy
Kidneys are retroperitoneal organs located between D12 and L3 vertebra. The right kidney is slightly lower than the left due to the presence of liver. It is also nearer to median plane when compared to the left.
Each kidney measures about 11 cm in length, 6 cm in width and 3 cm in thickness. It weighs between 125 to 170 grams in adult males and 115 to 155 grams in adult females.
Concave side of each kidney is indented by hilum through which renal artery, vein and ureter enters the kidney. Suprarenal (adrenal) gland is related to the upper pole of kidney.
Each kidney is surrounded by:
- Renal fascia of Gerota—it has two layers
- Anterior layer—fascia of Toldt
- Posterior layer—fascia of Zuckerkandl
- Perirenal fat in the space of Gerota
- Renal capsule around kidney which can be easily stripped off.
Cross-section of each kidney (Fig. 1.1) reveals:
- Cortex: This is the outer portion between the capsule and medulla. It has number of projections (cortical columns of Bertini) extending between the pyramids. It contains renal corpuscles and tubules.
- Medulla: This is the innermost part that consists of renal pyramids. This is further divided into:
- Inner medulla
- Outer medulla
- Renal papilla: It drains urine from medullary pyramids into minor calyx.
- Renal sinus: This is a space extending from renal hilum containing branches of renal artery and vein and renal pelvis
- Renal pelvis: A funnel shaped dilated upper part of ureter. It divides into 2–3 major calyces which further divides into 7–13 minor calyces.
Blood Supply
Blood supply of the kidney is derived from renal arteries. It arises from aorta at the level of L1-L2 intervertebral disc. Figure 1.2 shows the blood supply of a kidney.
Flow of blood in arterial side is as follows:
Segmental arteries → Lobar arteries → Interlobar arteries → Arcuate arteries → Interlobular artery (also known as cortical radiate arteries) → Afferent arterioles → Glomerulus.
Venous blood flows in following direction:
Glomerulus → Efferent arterioles → Interlobular vein → Arcuate vein → Interlobar vein → Renal vein.
Nerve Supply
Nerve supply to kidneys is through the renal plexus. Its fibers course along the renal arteries to reach the kidneys.
- Sympathetic input: Causes vasoconstriction thereby reducing renal blood flow
- Parasympathetic input: Through renal branches of vagus nerve
- Sensory input: Travels to spinal cord level T10-11.
MICROSCOPIC ANATOMY: THE NEPHRON
This is the basic functioning and structural unit of a kidney. It derives its name from Greek word nephros meaning kidneys. There are about 1.2 million nephrons in each kidney.
Nephrons form urine by process of filtration, secretion and reabsorption. It also functions to control blood pressure, red blood cell production and active vitamin D (calcitriol) synthesis.
As shown in Figure 1.3, each nephron is composed of:
- Renal corpuscle (the filtering unit): Formed by glomerulus and Bowman's capsule
- Renal tubule: Comprising of proximal convoluted tubule (PCT), loop of Henle with its ascending and descending limbs and distal convoluted tubule (DCT).
There are two types of nephrons:
- Cortical: Renal corpuscle of these nephrons are in cortex and loop of Henle located near corticomedullary junction.
- Juxtamedullary: Renal corpuscle of these nephrons are located in cortical part nearing medulla and loop of Henle is located deep in medulla.
Renal Corpuscle
It consists of glomerulus, which is surrounded by Bowman's capsule (Fig. 1.4). Bowman's capsule transfers the filtrate of glomerulus to the PCT. Bowman's capsule has an outer parietal layer, which continues onto the glomerular capillaries to form the inner visceral layer. Visceral layer is composed of visceral epithelial cells also known as podocytes, which covers the extensive capillary network, by its extension known as pedicles. Pedicles interdigitate to form sieve like filtration. The endothelium of glomerular capillaries, the glomerular basement membrane and the podocytes form the filtration barrier.
Most substance less than 8 nm and all the substances less than 4 nm can pass through the filtration barrier. Apart from this size barrier other factor determining the filtration across the filtration barrier is charge of a particular substance.
The negatively charged proteins associated with the pore repel, and thereby reduce, the filtration of negatively charged substance.
Mesangium is a thin membrane that supports the capillary loops. It is surrounded by capillaries. Mesangial cells are phagocytic cells located between the capillaries. These cells also contract to regulate the filtration rate.
Juxtaglomerular Apparatus
The juxtaglomerular (JG) apparatus lies just outside the glomerulus and Bowman's capsule as seen in Figure 1.5. It consists of:
- Macula densa: The initial part of DCT comes into contact with arterioles near the vascular pole of glomerulus. The wall of DCT at this point is formed by a specialized cluster of cuboidal epithelial cells known as macula densa, which monitors the composition of fluid passing through the DCT. These cells sense the changes in sodium chloride levels in distal tubule of kidney and release paracrine signals to regulate the flow.
- Juxtaglomerular cells: These are modified smooth muscle cells that line the media of afferent arterioles. The ATP or adenosine secreted by macula densa leads to contraction or relaxation of these cells, thereby regulating the glomerular blood flow. It also releases renin in response to various stimuli such as decreased NaCl concentration at macula densa, stimulation of beta1 adrenergic receptor and decreased renal perfusion pressure.
- Extraglomerular mesangial cells: The JG apparatus plays an important role in regulation of fluid balance of the body and helps in autoregulation.
Renal Tubules
Proximal Convoluted Tubule
It is the longest part of the renal tubule and the first one to receive the fluid filtered by Bowman's capsule. It is lined by simple tall cuboidal epithelium.
There are numerous microvilli on the apical surface of these cells, which considerably increase the surface area for reabsorption and secretion; two important functions of PCT. PCT cells contain numerous mitochondria due to high-energy requirements.
Henle's Loop
PCT continues as Henle's loop. It has following parts:
- Descending limb—this consists of:
- Initial short thick portion (pars recta): It has simple cuboidal epithelium like PCT
- Long thin portion: This has simple squamous epithelium
- Hairpin turn
- Ascending limb—this consists of:
- Short thin portion: Containing simple squamous epithelium
- Long thick portion: It has simple cuboidal epithelium like DCT.
They have different water and solute permeabilities, which play role in diluting and concentrating the urine by countercurrent mechanisms, which will be described later in section on physiology.
Distal Convoluted Tubule
It is tortuous like PCT and contain similar simple cuboidal cells but with fewer microvilli on the apical surface. It contains lesser number of mitochondria compared to PCT.
Collecting Duct System
Technically speaking this is not a part of the nephron. Each collecting duct drains several nephrons. Collecting duct can be divided into cortical and medullary part, while the medullary part is further divided into inner and outer segments. Medullary collecting ducts end at renal papilla. It has both cuboidal and columnar epithelium (near the papilla). There are two types of cells in collecting ducts – the intercalated and principal cells, which will be described in detail in section on physiology.
The squamous epithelium of collecting duct has receptors for anti-diuretic hormone (ADH). On stimulation of these receptors by ADH, aquaporins (the water channels) get inserted into the cell membrane and allow water to pass from lumen into the interstitial space. In the absence of ADH, dilute high volume urine is formed.
SECTION B: RENAL PHYSIOLOGY AND URINE FORMATION
INTRODUCTION
Having gone through the anatomical details of the kidneys, it's the time to proceed to the physiology of urine formation.
Kidney uses three key steps in urine formation:
- Filtration: This happens in the renal corpuscles where a filtrate is formed out of the blood passing through the glomerulus. This filtrate passes through the tubular system where its composition is altered by reabsorption or secretion leading to eventual formation of urine.
- Reabsorption: This involves transport of water, important ions and minerals (such as glucose, amino acids, sodium, potassium, magnesium, etc.) from the filtrate in the tubular lumen back into the blood surrounding the renal tubules.
- Secretion: This is a process by which various substance are transported into the tubular filtrate from the blood surrounding the tubules.
GLOMERULAR FILTRATION RATE AND PRESSURE
Kidney receives about one fifth of the blood pumped by the heart every minute (cardiac output). This blood is filtered to form about 125 ± 15 mL of filtrate every minute in men and about 110 ± 15 mL/min in women. Hence, a normal functioning kidney has a glomerular filtration rate (GFR) of about 180 L/day in men and 150 L/day in women.
The pressure that drives the filtrate out of the glomerular capillaries into the tubular lumen is known as the glomerular filtration pressure or net filtration pressure. This is determined by the forces favoring (hydrostatic pressure in glomerular capillaries i.e. PG) and opposing (hydrostatic pressure in Bowman's capsule i.e. PB and oncotic pressure exerted by plasma in glomerular capillaries i.e. OG) the flow. The oncotic pressure in Bowman's capsule is negligible.
Clearance of any substance is defined as volume of plasma, which gets completely cleared off of a substance per unit time.
Determination of GFR is an important step in assessment of renal function. There are various methods of GFR estimation. The gold standard is inulin clearance. Inulin is a polysaccharide that is neither reabsorbed nor secreted by the kidneys. Assessment of GFR by inulin requires intravenous administration of this drug. Method of inulin clearance is cumbersome; hence, an endogenous molecule serum creatinine is used to assess GFR in day-to-day clinical practice.
TRANSPORT MECHANISMS
There are various mechanisms by which substances are transported across membranes. These include:
- Active transport: This involves movement of molecules from lower to higher concentration across a cell membrane. As the movement is against the concentration gradient, this requires energy, which is usually derived form adenosine tri-phosphate (ATP)
- Diffusion: Simple diffusion involves movement of molecules down the concentration gradient, i.e. from higher to lower concentration.
- Facilitated diffusion: Here the molecules move from higher to lower concentration but require specific transmembrane proteins.
- Secondary active transport: Here the substance is moved in energetically unfavorable direction against the gradient facilitated by co-transport of another molecule down the gradient. These are of two types
- Symport: Two or more substances move in same direction.
- Antiport: Substances move in opposite direction across the cell membrane.
- Osmosis: This involves movement of solvent from the region of lower solute concentration to higher solute concentration across a semi-permeable membrane.
These mechanisms are involved in the process of reabsorption and secretion in renal tubules leading to the formation of urine.
TUBULAR TRANSPORTS
Proximal Convoluted Tubule
PCT is an important site for reabsorption of most of the water, electrolytes such as sodium, potassium etc. and organic solutes such as glucose and amino acids (Table 1.1). There are many channels present in the cells of PCT to facilitate the movement of various substances across the cell membrane. The Na+K+ ATPase pump present in the basolateral membrane actively transports Na out of the cell creating a gradient across the cell membrane leading to sodium reabsorption. This is an energy driven process. Reabsorption of Na is coupled with the movement of various substances either in the same (symport) or the opposite (antiport) direction (Fig. 1.6). Table 1.2 shows substances transported across the apical and basolateral membrane of PCT.
9
|
Carbonic anhydrase (CA) is an important enzyme located inside the PCT cells. It is also present on the cell surface in small amount. In the tubular lumen, HCO3− combines with H+ to form H2O and CO2 in presence of CA. CO2 diffuses into the cell. Here the reverse reaction occurs, in presence of CA, leading to the formation of HCO3− and H+. HCO3− is cotransported with Na across basolateral membrane and apical Na/H antiporter secretes H+ back in the lumen. This process recovers the bicarbonate.
10
There are few substances secreted in PCT. Most of the drugs are secreted here. These include furosemide, indomethacin, penicillin, and probenecid to name a few. Apart from this PCT is the site for formation of most of the ammonia secreted in urine.
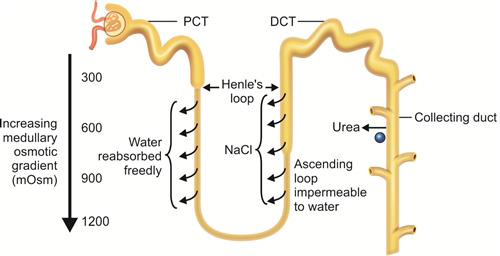
Loop of Henle and the Countercurrent Mechanism
The Henle's loop functions to reclaim the solute and water from the filtrate. As discussed in the section on anatomy, Henle's loop has two limbs:
- Descending limb: This has aquaporin channels, which lead to free movement of water from tubular lumen to the interstitium leading to about 15–20% reabsorption of water. This happens because of the increasing interstitial osmolarity as one descends down the limb. Some amount of urea, sodium and other ions are also reabsorbed.
- Ascending limb: Na+K+ ATPase present in basal surface leads to extrusion of sodium outside the cell. This creates a Na+ gradient. Ascending limb cells are impermeable to water but rich in Na+K+2Cl– channels (Fig. 1.7). Sodium moves down the gradient and potassium along with chloride is transported along with it. tubular fluid leaving the ascending limb to enter DCT is hypoosmotic (100 mOsm/kg).
Interstitial osmolarity increases from 300 mOsmol/kg to 1200 mOsmol/kg as one moves from corticomedullary junction to medulla. Apart from the sodium reclaimed by ascending tubule by Na+K+2Cl– channels and Na+K+ ATPase described above, facilitated diffusion of urea from inner medullary collecting ducts into the medullary interstitium add to produce high medullary osmolarity. This happens due to the countercurrent multiplier mechanism. The name countercurrent multiplier exchange is derived from countercurrent arrangement of the two limbs of Henle's loop leading to flow of tubular filtrate in opposite directions (Fig. 1.8).
Due to the above arrangement the medullary interstitium becomes hyperosmotic (almost 1200 mOsm/kg at the tip). This facilitates the water movement across the descending limb as described leading to concentration of tubular filtrate.
Further, the presence of vasa recta serves as a countercurrent exchangers to prevent the solute washout from the hyperosmotic interstitium. This is also helped by the low medullary blood flow (<5% of total renal blood flow).
Distal Convoluted Tubule
The DCT functions to recover water and various solutes from the hypotonic fluid reaching it. Various channels of DCT play significant role in this (Fig. 1.9).
- The basal Na+K+ ATPase channel of DCT moves Na out of the cell creating gradient for
- Na to be absorbed from the apical Na/Cl symporter
- Ca reclamation by Na/Ca antiporter in basolateral membrane
- Up to 10–15% of total filtered water reabsorption
- About 7–10% of filtered calcium is reabsorbed via transcellular route by TRPV5 channel
- Basal transport of calcium also occurs via calcium ATPase
- Magnesium is reabsorbed by TRPM6 apical channel
- Regulation of sodium and potassium levels by apical ENaC (sodium reabsorption) and ROMK (potassium excretion) channels.
Collecting Duct
Collecting duct drains urine from the DCTs. It serves an important function in formation of diluted or concentrated urine. It also helps in sodium, potassium and acid-base regulation.
- Urine volume and osmolarity regulation: Antidiuretic hormone (ADH) (vasopressin) is the hormone responsible for regulation of urine volume and osmolarity. It leads to insertion of aquaporin channels into the apical membrane of principal cells lining the collecting duct. Water is reabsorbed through these aquaporin channels because of the increasing interstitial osmolarity as the collecting duct traverses the medulla. In case blood becomes hyperosmotic, more water is reabsorbed by above-mentioned ADH action. In case blood is hypoosmotic, opposite occurs, leading to formation of dilute urine.
- 13Sodium and potassium homeostasis by principal cells: An important hormone, aldosterone, stimulates luminal Na and K channel formation as well as the activity of basal Na/K ATPase pump (Fig. 1.10A). In case of increase in serum aldosterone, more sodium is reabsorbed and potassium is lost in urine. Water is reabsorbed as well.
- Acid-base balance by intercalated cells: There are two types of intercalated cells which are mirror images of each other (Figs 1.10B and C)
- α intercalated cells: Secretes H+ ion and reabsorbs bicarbonate
- β intercalated cells: Secretes bicarbonate ion and reabsorbs H+Damage to these cells can lead to renal tubular acidosis.
AUTOREGULATION
Renal blood flow remains relatively stable to maintain a normal GFR over a wide range of blood pressure (mean arterial pressure of 70–160 mm Hg). This is known as autoregulation and has two important components:
- Myogenic response: The afferent arteriole wall smooth muscle cells are stretched when BP increases. It contracts in response to this, leading to little change in blood flow. The opposite happens when BP drops.
- Tubuloglomerular feedback (TGF): Important components of TGF are juxtaglomerular apparatus (JGA) and a paracrine signaling mechanism. Macula densa cells of DCT respond to the flow of tubular filtrate as well as sodium and chloride concentration of the filtrate. Increasing GFR leads to increase in tubular flow. Macula densa detects it and releases ATP and adenosine. These lead to contraction of the juxtaglomerular (JG) cells of afferent arterioles thereby reducing GFR. Drop in GFR has the opposite effect.
Other important mechanisms involved in controlling the effective circulatory volume include sympathetic nervous system and renin-angiotensin-aldosterone system (RAAS).
SYMPATHETIC NERVOUS SYSTEM
Kidneys receive the sympathetic supply from the celiac plexus and the splanchnic nerves. Reduced effective circulatory volume results in reflex increase in sympathetic nerve discharge leading to vasoconstriction and reduced glomerular flow and filtration. This also leads to stimulation of renin secretion. Renin further leads to circulatory volume augmentation as described below.
RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM (RAAS)
Decrease in renal perfusion leads to secretion of renin by granular cells of afferent arteriole at the JGA. It converts angiotensinogen derived from liver to angiotensin I. This is further converted by angiotensin converting enzyme (ACE) to angiotensin II. This enzyme is produced in lungs and binds to endothelial cells of afferent arteriole and glomerulus (Fig. 1.11).
Angiotensin II has multiple effects by which it tries to maintain blood volume and pressure such as:
- Increased sympathetic activity leading to afferent and efferent vasoconstriction and preservation of blood volume.
- Direct systemic arteriolar vasoconstriction leading to increased blood pressure
- Promotes secretion of aldosterone from adrenal cortex. This leads to sodium reabsorption and potassium excretion. This also leads to reabsorption of water along with sodium.
- Secretion of ADH leading to fluid retention.
ENDOCRINE FUNCTION OF KIDNEYS
Apart from its role in RAAS and ADH mediated fluid regulation there are few other important endocrine functions of kidney worth mentioning here:
- Erythropoiesis: Kidney secretes erythropoietin hormones in response to hypoxia. It is secreted by renal cortical interstitial cells near the base of PCT. Kidneys account for about 85% secretion of EPO. In chronic kidney disease, deficiencies of these hormones lead to anemia requiring EPO supplementation.
- Active vitamin D (calcitriol) synthesis: Active form of vitamin D i.e. 1,25-dihydrocholecalciferol also known as calcitriol is synthesized in the renal PCT. The enzyme 1-alpha-hydroxylase acts on its substrate 25-hydroxycholecalciferol leading to the formation of active vitamin D.
SUMMARY
- Kidney performs important function of maintaining fluid, electrolytes and acid-base balance in the body.
- It also secretes important hormones such as active vitamin D3 and erythropoietin and has an important role to play in the regulation of blood pressure.
- Compromise of these functions leads to various manifestations of renal failure, which may be fatal.
- Understanding of the basic renal anatomy and physiology is important for management of patients with renal dysfunction.
1. Kidney has following function:
- Excreting waster product
- Secreting hormones
- Regulating acid base balance
- All of the these
2. The average numbers of nephrons per kidney is:
- 1.2 lakh
- 1.2 million
- 2.4 million
- 12 million
3. Macula densa cells are:
- Extraglomerular mesangial cells
- Cluster of cuboidal epithelial cells forming wall of DCT where it comes in contact with the arterioles
- Modified smooth muscle cells lining media of afferent arterioles
- None of the above
4. Which one of the following about flow of renal blood supply is correct?
- Lobar arteries → Segmental arteries → Interlobar arteries → Arcuate arteries → Afferent arterioles
- Segmental arteries → Arcuate arteries → Lobar arteries → Interlobar arteries → Afferent arterioles
- Segmental arteries → Lobar arteries → Interlobar arteries → Arcuate arteries → Afferent arterioles
- None of the above
5. Filtration barrier is formed by:
- Endothelium of glomerular capillaries
- Glomerular basement membrane
- Podocytes
- All of the above
6. Average net filtration pressure is:
- 5 mm Hg
- 10 mm Hg
- 25 mm Hg
- 100 mm Hg
7. Gold standard for GFR determination is:
- DTPA renal scan
- eGFR by Cockcroft Gault formula
- Inulin clearance
- eGFR by MDRD formula
8. Glucose is absorbed completely in:
- Distal convoluted tubule
- Proximal convoluted tubule
- Loop of Henle
- Collecting duct
9. Angiotensin converting enzyme is synthesized in:
- Liver
- Lungs
- Kidneys
- All of these
10. Collecting duct functions to:
- Maintain urine volume and osmolarity
- Sodium and potassium homeostasis
- Acid-base balance
- All of the above
1. d | 2. b | 3. b | 4. c | 5. d | 6. b | 7. c | 8. b |
9. b | 10. d |
SUGGESTED READING
- Bailey MA, Shirley DG, Unwin RJ, Renal physiology. In: Johnson RJ, Feehally J, Floege J (Eds). Comprehensive Clinical Nephrology, 5th edn. Elsevier/Saunders. Philadelphia, PA: 2015. pp.14–27.
- Barajas L. Anatomy of the juxtaglomerular apparatus. Am J Physiol. 1979:237(5): F333–43.
- Barrett KE, Barman SM, Boittano S, Brooks HL, Renal physiology. In: Barrett KE, Barman SM, Boittano S, Brooks HL (Eds). Ganong's Review of Medical Physiology, 23rd edn. McGraw-Hill Medical. New York,: 2010. pp. 639–86.
- Blaine J, Chonchol M, Levi M. Renal control of calcium, phosphate, and magnesium homeostasis. Clin J Am Soc Nephrol. 2015:10(7):1257–72.
- Danziger J, Zeidel. Osmotic homeostasis. Clin J Am Soc Nephrol. 2015:10(5): 852–62.
- Healy JC. Urogenital system. In: Standring S (Ed). Gray's Anatomy: The Anatomical Basis of Clinical Practice, 41st edn. Elsevier. Philadelphia: 2015. pp. 74–8.
- Kriz W, Elger M. Renal anatomy. In: Johnson RJ, Feehally J, Floege J (Eds). Comprehensive Clinical Nephrology, 5th edn. Elsevier/Saunders. Philadelphia, PA: 2015. pp. 2–13.
- Subramanya AR, Ellison DH. Distal convoluted tubule. Clin J Am Soc Nephrol. 2014;9(12):2147–63.